
 We have recently made some important progress in researching the Edgar
Cayce information on epilepsy. In over two hundred readings Cayce discussed
the causes and treatment of epilepsy, most often citing problems in the
peripheral nervous system as a primary cause of epilepsy. Specifically,
aberrant nerve impulses coming from the abdomen to the head were frequently
noted as triggering seizures in the brain.
We have recently made some important progress in researching the Edgar
Cayce information on epilepsy. In over two hundred readings Cayce discussed
the causes and treatment of epilepsy, most often citing problems in the
peripheral nervous system as a primary cause of epilepsy. Specifically,
aberrant nerve impulses coming from the abdomen to the head were frequently
noted as triggering seizures in the brain.
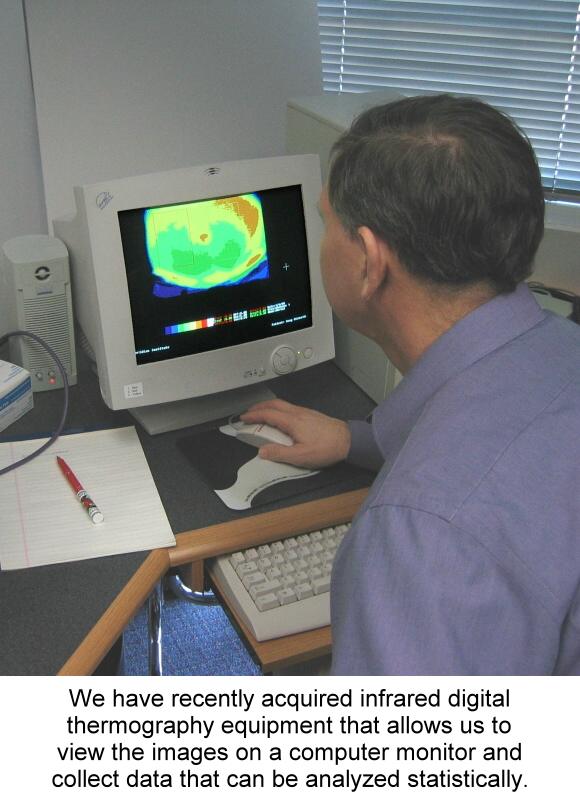
The pathology in the abdomen was linked to a unique pattern of thermal variation on the surface of the skin. Cayce stated that, "From EVERY condition that is of true epileptic nature there will be found a cold spot or area between the lacteal duct and the caecum." (567-4) The lacteal duct and caecum are on the right side of the abdomen just below the last rib and extending down to the point of the hip. This statement represents a very straightforward hypothesis that can be tested using modern thermographic equipment. We have collected some preliminary data on abdominal thermographic patterns using liquid crystal thermography. We discussed this preliminary stage of our epilepsy research program in a previous issue of this newsletter (Vol. 4, No. 5). The data is promising, but limited from a scientific standpoint because the technique only yields colored Polaroid pictures that do not lend themselves to the type of statistical analysis required for scientific proof. We have recently obtained a more sophisticated infrared camera that yields color images and statistical data (See photo). Although this equipment is currently on lease, due to the generosity of a private donor, we will be purchasing an even more modern model for use in the next phase of our epilepsy research program. The Abdominal Brain The obvious question that arises in researching this
Cayce hypothesis on epilepsy is, "How can a cold spot on the abdomen have
anything to do with seizures in the brain?" In reviewing the historical
and modern literature, we believe that we have uncovered some important
clues to understanding Cayce's model.
The abdominal brain exchanges information with the cerebral brain via the vagus nerve. About seventy percent of the nerve impulses that are transmitted along the vagus go from the abdomen to the brain. Thus the abdomen is a significant source of nerve impulses to the brain. We believe that impulses traveling along the vagus nerve from the abdomen to the head could be the source of seizures in some epilepsy patients. The technical term for such seizures is "visceral reflex epilepsy." Visceral Reflex Epilepsy The next stage of our epilepsy research program will explore the plausibility of the concept of visceral reflex epilepsy. The specific aim of the project is to compare abdominal thermographic data to patient history data of epilepsy patients with various forms of epilepsy to determine whether our preliminary findings are valid and can be translated into innovative clinical interventions. Reflex epilepsy includes a group of epileptic syndromes in which seizures are induced by a stimulus. The stimulus may be simple (e.g., visual, somatosensory, olfactory, auditory) or complex (e.g., eating, thinking, reading). Most cases of documented reflex epilepsy are diagnosed because the triggering stimulus is easily identified. The hypothesis that we are testing in our project is based on the premise of a broader conceptualization of reflex epilepsy to include visceral stimuli that are not as obvious as typical reflex seizure precipitants. Visceral symptoms that precede seizures (premonitions) or occur during the early stages of the seizure itself (aura) are common and suggest autonomic nervous system (ANS) involvement at some level. Although it is usually assumed that ANS involvement is an effect of primary central nervous system (CNS) pathology, some researchers have suggested that ANS involvement may have etiological significance. Thus, visceral symptoms may be associated with underlying visceral processes that act as precipitating factors in some cases of epilepsy. Abdominal epilepsy is diagnosed when the visceral symptoms predominate. Perhaps abdominal pathophysiology is more widespread in epilepsy than is generally conceived. As mentioned above, the vagus nerve is a primary neural pathway between the viscera and the brain. The use of vagus nerve stimulation treatment for epilepsy may be indicative of interruption of the reflex pathway between the viscera and brain. Research Methodology Epilepsy patients will be recruited and matched with normal controls for evaluation of abdominal thermographic patterns. The epilepsy patients will also complete symptom inventories intended to assess the presence and severity of abdominal symptoms. Thermography of the surface of the abdomen will be performed using an infrared camera. Digital imaging software will be used to quantify the temperature patterns as a measure of autonomic vasomotor activity in terms of average temperatures in selected areas, and of temperature differentials. There will be intra-individual comparisons of the left and right sides of the abdomen, correlated with the side of the focus for partial seizures, as well as a comparison of the epileptics with the controls. The project involves no treatment intervention. "You Will Be Undefeatable" Epilepsy research is a high priority for us.
One of the motivations for this emphasis comes from another quote from
the Cayce readings, ". study on that called epilepsy - for THREE YEARS!
And you will be undefeatable!" (254-82) You can see why we
are so excited about this project. Stay tuned for more in the months
ahead!
CASTOR OIL PACK STUDY REPORT Meridian Institute recently completed a pilot study on abdominal castor oil packs. The specific aim of the research project was to evaluate the effect of castor oil packs over the right side of the abdomen on laboratory measures designed to assess the liver's detoxification capability. It was intended as a small trial to collect preliminary data. Castor oil has a long tradition of use in folklore medicine. In the early 20th century, Edgar Cayce recommended castor oil packs as an external application over the right side of the abdomen for a variety of conditions. These were intended to help increase eliminations, stimulate the liver and gallbladder, and dissolve adhesions. In our study, ten subjects (5 experimental and 5
control) participated in the project to test the effect of castor oil packs
on three measures of liver function: processing of caffeine, aspirin, and
acetaminophen. The members of the experimental group used castor oil packs
(flannel saturated with castor oil and warmed by a heating pad) over the
liver for 3 days, 1 hour per day. The members of the control group used
dry flannel warmed by a heating pad. Saliva and urine samples were taken
to be tested for liver function before and after the 3-day process, and
analyzed by the Great Smokies Diagnostic Laboratory. There were no significant
differences between the pre and post samples for any of the measures of
liver function, nor were there differences between the experimental and
control groups. Possible explanations include: (1) no effect of castor
oil packs on liver function, (2) low reliability of some of the tests,
(3) inadequate exposure to the castor oil packs for an effect to be measured.
MEDITATION FOR IBS The Relaxation Response Meditation (RRM) program developed by Herbert Benson over twenty-five years ago has been shown to be helpful for irritable bowel syndrome (IBS). Two studies conducted by researchers at the Center for Stress and Anxiety Disorders (State University of New York at Albany) indicate that a six week course of RRM decreases symptoms in both the short- and long-term. Thirteen of sixteen IBS patients in the initial study completed the six week program after being matched into pairs and randomized to either a six week meditation group or a six week wait list. All subjects assigned to the Wait List were subsequently treated. Patients in the treatment condition were taught the meditation technique and asked to practice it twice a day for 15 minutes. By three month follow-up, significant improvements in flatulence (P<0.01), belching (P=0.02), bloating (P=0.05), and diarrhea (P=0.03) were shown by symptom diary. Constipation approached significance (P=0.07). Ten of thirteen original subjects also participated in a one year follow-up study to determine whether the effects of RRM were maintained over a longer term. From pretreatment to one-year follow-up, significant reductions were noted for the symptoms of abdominal pain (p = 0.017), diarrhea (p = 0.045), flatulence (p = 0.030), and bloating (p = 0.018). The researchers concluded that RRM is a beneficial treatment for IBS in both the short- and the long-term. References Keefer L, Blanchard EB. The effects of relaxation response meditation
on the symptoms of irritable bowel syndrome: results of a controlled treatment
study. Behav Res Ther 2001 Jul;39(7):801-11.
|
